Central station setup with bridge and dashboard.
Designing AI tools for nurse support
This project explores the integration of AI technologies in healthcare, focusing on the challenges nurses face in managing cognitive load, building trust, and improving communication. A field study at Norrlands Universitetssjukhus highlighted concerns about AI autonomy, decision-making transparency, and information overload. Based on these findings, the project proposes a dashboard solution that reduces information overload, enhances collaboration, and ensures transparent AI support, empowering nurses to maintain control over clinical decision-making. By prioritising human expertise while tapping into AI to support clinical decisions, the solution aims to reduce the cognitive burden on nurses, improve workflow efficiency, nurse well-being, and ultimately patient care. This research offers a framework for designing AI systems that complement, rather than replace, healthcare professionals’ judgment and expertise.
Introduction
Healthcare systems worldwide are under immense strain due to rising patient numbers, complex cases, and aging populations. These pressures, compounded by staff shortages, increase stress and cognitive demands on medical professionals, threatening their well-being and career longevity. Innovative solutions are urgently needed to maintain care quality and support staff in their roles.
Telehealth monitoring has emerged as a promising approach to address these challenges by integrating technology into care workflows. By redistributing workloads and enhancing patient safety, telehealth has the potential to ease the burden on nurses. This design brief explored how telehealth solutions could empower nurses by supporting decision-making, reducing cognitive load, and improving crisis management. Through a six-week interaction design project in collaboration with Philips Healthcare, a humancentered approach was taken to address these issues. Conversations with medical designers and nurses highlighted both the potential of AI and automation and the skepticism surrounding its impact. Concerns included reduced transparency, loss of control, over-reliance on technology, and erosion of intuition: qualities nurses expressed as critical to patient care. In response, our team focused on trust as a core theme, narrowing its scope to nurses at central monitoring stations in postoperative wards. These stations enable telehealth nurses to monitor patient vitals remotely and collaborate with bedside staff. By targeting this touchpoint, the project aimed to enhance workflow efficiency while exploring how trust in technology can be built and sustained.
Methodology
Our project utilized a user-centered design approach to explore trust and efficiency in integrating AI into healthcare settings. The methodology was rooted in understanding the lived experiences of nurses and the environments they navigate today. Our method emphasized empathy and collaboration, ensuring solutions aligned with real-world needs while addressing the complexities of trust and efficiency.
Field Research: We began with a day of field visit to Norrlands universitets sjukhus, including Thorax, AnOpIva, and ICU units, engaging directly with nurses to observe workflows and challenges in their natural settings. This provided first-hand insights into their work environment and highlighted critical pain points, such as alarm fatigue and cognitive burden.
Ethnographic Storytelling: To humanize our findings, we crafted relatable stories using ethnographic storytelling templates. These narratives preserved the emotional and procedural aspects of the nurses’ experiences, enabling us to focus on themes such as trust in technology, collaboration, and learning.
Scenario Prototyping: We developed three future scenarios of technological integration, ranging from minimal intervention to fully immersive technologies. These scenarios enabled discussions among nurses, Philips representatives and classmates about the benefits, risks, and implications of varying levels of technological involvement in healthcare. From this we identified trust dimensions such as transparency, reliability, consent, and collaboration.
Workflow: We analyzed the existing nursing workflow at NUS to identify pain points, particularly around communication, cognitive load, and trust in technology. Using these insights, we reimagined the workflow to incorporate a central station nurse and telehealth tools. This redesigned workflow served as a foundation for conceptualizing AI-powered designs like MAIA. By mapping tasks and interactions, we prototyped user interfaces to seamlessly integrate AI, focusing on minimizing disruptions and maintaining nurse autonomy. Iterative testing ensured the designs aligned with the workflow’s needs, enhancing collaboration, reducing alarm fatigue, and fostering trust in the new system.
Result
The project resulted in a comprehensive dashboard concept designed to streamline workflows for nursing staff at the central station. By integrating patient data, AI insights, and communication tools, the dashboard provides a customizable and supportive solution aimed at reducing cognitive load and improving efficiency during quieter moments in a nurse’s shift. These quieter moments, often overlooked, present an opportunity to enhance decision-making and prevent future crises, ultimately reducing stress during high-pressure situations. The dashboard features three main sections: patient history, AI system MAIA, and detailed monitoring, with an additional alarm and communication panel. MAIA assists nurses by offering transparent, evidence-based recommendations without overriding their autonomy, thus fostering trust. The system is designed to enhance collaboration between central station and bedside nurses, allowing for timely intervention, such as when MAIA identifies potential risks like sepsis or issues with post-operative pain management. The concept was evaluated through detailed user flows, demonstrating how the dashboard could support nurses in specific scenarios. In one flow, MAIA suggests a medication adjustment for post-operative pain, while in another, it identifies a potential sepsis risk based on continuous monitoring of vital data. These scenarios highlighted how MAIA can reduce cognitive load and support nurses' decisionmaking without undermining their professional judgment. The dashboard optimizes workflows, enhances nurse autonomy, and fosters trust in AI-assisted decision-making, addressing both operational challenges and nurse well-being.
Jonatan Wickström
Sarah Mai Eigel
Signe Lindgren
Concept video

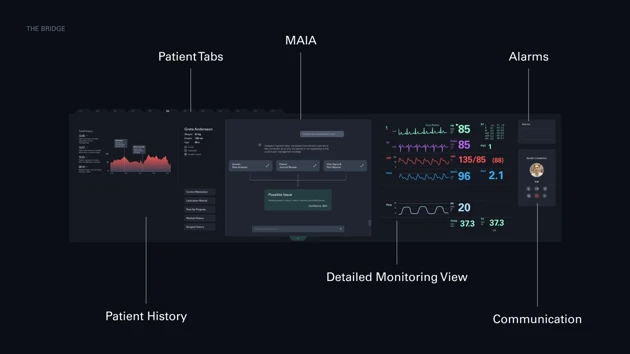
Interface: The dashboard
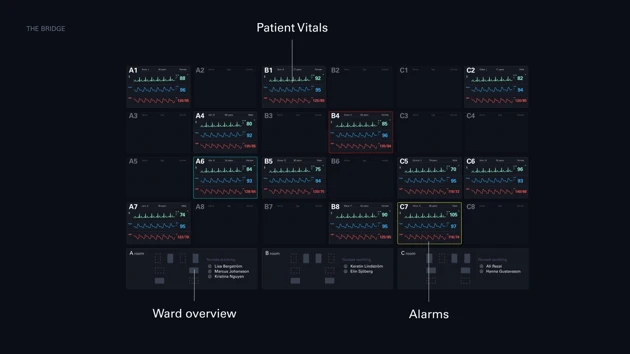
Interface: The bridge
Ideation: Crazy eights

Field trip: Thorax ward






